What is a Caesarean Section?
The common reasons for having a caesarean section are:
- A previous caesarean section.
- Low lying placenta.
- Breech presentation.
- Multiple pregnancy.
- High blood pressure.
- Baby not growing at the expected rate.
There are many other reasons that you and your obstetrician may decide that a caesarean section is preferable for the delivery of your baby. If you have any questions you should ask your obstetrician.
Before the Operation (Admission to Hospital for a Caesarean Section)
- Usually you may bring a camera in the operating room, to take photos of your baby as soon as he or she is born. However in most hospitals video is not allowed.
- The day of surgery. No food or drink for 6-12 hours prior to surgery.
- You will also meet your anaesthetist prior to the surgery.
- You may be asked to drink an antacid medication just prior to surgery.
In the Operating Room (Anaesthesia)
- You will be given an anaesthetic so that you do not feel the surgery.
- The anaesthetic will be with you at all times.
There are 2 types of anaesthesia:
1. Regional anaesthesia
2. General anaesthesia
If you have any questions about your anaesthetic you should ask your obstetrician and anaesthesstist.
In the Operating Room (Regional Anaesthesia)
- If you have a regional anaesthesia, you will be awake.
The types of regional anaesthetic available for a caesarean section are:
- Spinal anaesthetic
- Epidural anaesthetic
An epidural anaesthetic is commonly used in labour. It may be topped up if a caesarean section becomes necessary.
In the Operating Room (General Anaesthetic)
- A general anaesthetic may be necessary if:
- There are difficulties with regional anaesthetic
- You have a serious bleeding tendency
- The caesarean section is expected to be very complicated.
- About 1 in 50 cesarean sections are performed under general anesthesia.
- A drip will be placed in your arm.
- You will not feel or be aware of the surgery.
In the Operating Room (The Surgical Team)
Also present in the Operating Room will be:
- The anesthetist
- The pediatrician and/or the Midwife and all the neonatal nurse.
- The Operating Room support staff.
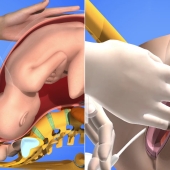
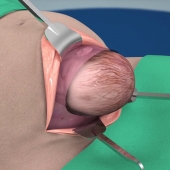
In the Operating Room (The Procedure)
You will have some awareness of pushing or pressure, feelings during the surgery but you will not feel anything sharp or painful. If you are at all uncomfortable you should tell your anesthetist.
In the Operating Room (Your Baby)
The umbilical cord will be clamped and cut. You'll be able to see your baby as soon as he or she is born.
The midwife all pediatrician will then place your baby on the resuscitation trolley to:
- Dry your baby
- Ensure your baby is breathing normally
- Ensure your baby has a good color and heart rate
- Trim the cord close to the umbilicus
- Give your baby vitamin K if you have given your approval
Your baby will be brought over to you to hold. You may have some skin-to-skin contact at this time. In some cases your baby may be able to stay with you and accompany you to the recovery room.
In the Operating Room (After the Operation)
The placenta is removed and the uterus checked to ensure it is empty. The skin closed with sutures or staples. A clean dressing is applied over the wound. Observations will be taken of your blood loss blood pressure pulse and temperature for a further 30 to 60 minutes. You may experience some cramps during this time or experience some nausea. Your legs will be numb for several hours after a regional anaesthetic.
What to Expect After a Caesarean Section (Catheter)
Occasionally the catheter may need to stay in longer. For example if there has been heavier than usual bleeding during the caesarean section.
What to Expect After a Caesarean Section (Intravenous Drip)
Occasionally, the drip may be needed for longer if there has been heavier than usual bleeding during the caesarean section or if intravenous antibiotics are needed.
What to Expect After a Caesarean Section (Pain Relief)
You wil be given pain killers during the post-operative period.
Usually:
- Long-acting narcotic strong painkillers and anti-inflammatory medications given orally.
Occasionally:
- Anti-inflammatory medication may be given rectally.
- Intravenous form of pain relief It is important that you take sufficient pain relief so that you are able to move around comfortably after the operation.
What to Expect After a Caesarean Section (Going Home)
Usually, you will be eating drinking moving comfortably and looking after your baby by day 3 after the surgery. Most women return home between day 3 and day 5 after a cesarean section.
What to Expect After a Caesarean Section (Short Term After Effects)
Complete healing of the wound takes approximately 6 weeks. No heavy lifting or strenuous exercise for 6 weeks. Vaginal bleeding may continue for up to 6 weeks. If your bleeding ever becomes heavy and bright red again, you should contact your doctor or hospital. Once the bleeding has settled, you may resume sexual intercourse. Check with your doctor and your car insurance company before you resume driving.
Risk of Caesarean Birth
All births involve small risks to the mother and baby. There are some risks that are slightly higher with cesarean birth and some risks that are slightly lower with cesarean birth. It is not possible in this education module to detail all the possible risks of a cesarean birth. We will discuss the major risks associated with cesarean birth. These risks may be higher or lower in your case, depending on the reason for your cesarean birth, and other risk factors you may have. It is very important to discuss with your doctor the individual risks to you of your cesarean birth.
Risk of Caesarean Birth (Bleeding)
For most women, there is no increased risk of excessive bleeding, or postpartum hemorrhage, with a planned cesarean birth compared to a planned virginal birth. The risk of blood transfusion for a planned caeserean birth is about 4 in 1000. In these situations, flood will routinely be cross-matched and available for your delivery. You should discuss the possible need for blood transfusion with your doctor.
Risk of Caesarean Birth (Damage to Surrounding Organs)
The risk of damage to these organs at planned cesarean section is approximately 1 in 100.
Organ damage may require:
- An increase in operating time.
- A larger abdominal incision than originally planned.
- Increased blood loss and need for transfusion.
- A longer recovery period and hospital stay.
Risk of Caesarean Birth (Infection)
It is important to tell your doctor if you notice:
- A fever
- Redness, swelling, bleeding or leaking a fluid from the wound
- Burning, stinging or frequent urination
- Excessive vaginal bleeding, which becomes bright and heavy, having previously been lighter and darker
Risk of Caesarean Birth (Blood Clots)
Treatment may require blood thinning drugs.
The duration of the treatment will depend on other risk factors such as:
- A family history of clots
- Your age
- Your weight
- If you are a smoker
You should discuss the need for blood thinning medication with your doctor.
Risk of Caesarean Birth (Breathing Difficulties for the Baby)
The risk of breathing difficulties is lower the more mature your baby is at the time of cesarean birth.
- 36921 views